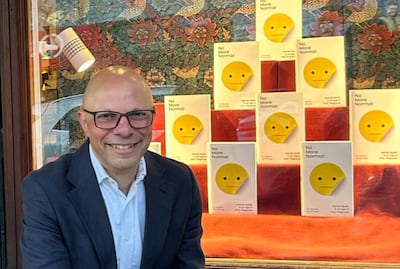
Alastair Santhouse’s recently published book No More Normal provides a window on to an experienced clinician’s thinking on mental health and exposes the fissures that exist within global debate about the subject.
The author suggests that as awareness of mental health has expanded, so has the propensity to overdiagnose, rather than accepting that what someone may be experiencing is the regular human condition. Over the course of almost 300 pages, he might well be saying that as the cadence of conversation around mental health has increased, we have reached a point where we are, in fact, talking too much.
“I have worried too long about the problem of diagnostic creep, whereby the category of normal is consistently eroded,” he writes. “What counts as a diagnosis and what counts as normal mental health are becoming more flexible. Increasingly, the concept of evidence is not decided by evidence but by social trends and appeals to emotion.
“We are now medicalising people who in previous generations would have been considered normal.”
Santhouse said in a recent Telegraph interview to promote the book that many of his patients suspect they have a mental illness but become upset when he tells them what they are experiencing fits within the range of normal.
In the book, the author cites a 2023 editorial in the Economist, provocatively titled “How to stop overmedicalising mental health”, which is clearly an influential reference point in his narrative, that concluded we should “avoid the mass medicalisation of mild forms of distress. All suffering should be taken seriously, but a diagnosis is not always in someone’s best interests”. Compassion carries us only so far forward, we need to be more thoughtful, too, it said.
In most parts of our lives, a significant part of a rise in diagnosis can be attributed to awareness and education rather than contagion
Returning to No More Normal, society has, Santhouse writes, “become increasingly one of self-care, which can tip into self-obsession. This is a recipe for trouble”.
He takes aim at depression by asking at what point does a normal level of sadness move over into a formal diagnosis, and he writes that where the two meet is hard to accurately delineate. And then, in his words, there is the “strange” and “muddled” history of trauma and PTSD, about which he says there is still no real consensus on what psychological trauma means. Adult ADHD was a diagnosis that “barely existed” a generation ago, he writes.
By now, his thesis will be clear to you: a propensity to want to define elements of our experience has led to a decline in the threshold of what is regarded as normal and to the emergence of a culture of overdiagnosis.
The more challenging aspect of that argument is that if we truly lean into the idea that this is the era of overdiagnosis, then we risk turning discussions about mental health into a form of generational war.
For decades, the misconceptions about mental health were discriminatory and derogatory. Poor mental health has often been seen as an incurable deficiency, a weakness or even a danger to society. Compare this to how society views a physical illness and the chances for success and recovery through rehabilitation. If we accept the overdiagnosing argument, we risk devaluing mental health discussions by saying what you thought was one thing is something far less consequential all together. In most parts of our lives, a significant part of a rise in diagnosis can be attributed to awareness and education rather than contagion.
Santhouse acknowledges that the shame around mental health (it is worth noting that the literal meaning for stigma, so often used to discuss the mental health landscape, is “a mark of disgrace”) has been in steady decline, but he caveats it by making the point that “progress in society changes the landscape of disease. Tell me what your diseases are and I will tell you what decade you are living in”.
So where does that leave us? First, read the book. It’s challenging and engaging – depending on your point of view, you will either strongly agree or completely disagree with his argument, which he supports by using anecdotes and evidence – but his words make it impossible to shake the feeling, for this writer at least, that this is a weaponisation of mental health after decades of hard-fought disarmament.
“Life can be hard and the hard parts are unavoidable. But life’s problems are a challenge to be overcome. They are not necessarily a sign of illness or disease,” he concludes.
Some of this news organisation’s work is in mental health. We run an in-country fellowship programme for journalists, in partnership with the Carter Centre in the US, who want training and mentorship and to be able to learn how to produce fair reporting on mental health. Much of the message we carry to those interested in working on mental health stories is to recognise how language shapes the conversation and the media’s responsibility in that endeavour, as well as to understand the importance of lived experiences, nuance, recovery, telling the whole story and recognising your own biases. We champion empathy but we also demand accuracy.
As the editorial on overmedicalising that I cited earlier concluded, we all need to be compassionate and more thoughtful in our complicated and complex world. To do so, we may need to reinterpret what “normal” really means.
Places to go for free coffee
- Cherish Cafe Dubai, Dubai Investment Park, are giving away free coffees all day.
- La Terrace, Four Points by Sheraton Bur Dubai, are serving their first 50 guests one coffee and four bite-sized cakes
- Wild & The Moon will be giving away a free espresso with every purchase on International Coffee Day
- Orange Wheels welcome parents are to sit, relax and enjoy goodies at ‘Café O’ along with a free coffee
Tax authority targets shisha levy evasion
The Federal Tax Authority will track shisha imports with electronic markers to protect customers and ensure levies have been paid.
Khalid Ali Al Bustani, director of the tax authority, on Sunday said the move is to "prevent tax evasion and support the authority’s tax collection efforts".
The scheme’s first phase, which came into effect on 1st January, 2019, covers all types of imported and domestically produced and distributed cigarettes. As of May 1, importing any type of cigarettes without the digital marks will be prohibited.
He said the latest phase will see imported and locally produced shisha tobacco tracked by the final quarter of this year.
"The FTA also maintains ongoing communication with concerned companies, to help them adapt their systems to meet our requirements and coordinate between all parties involved," he said.
As with cigarettes, shisha was hit with a 100 per cent tax in October 2017, though manufacturers and cafes absorbed some of the costs to prevent prices doubling.
Januzaj's club record
Manchester United 50 appearances, 5 goals
Borussia Dortmund (loan) 6 appearances, 0 goals
Sunderland (loan) 25 appearances, 0 goals
How much do leading UAE’s UK curriculum schools charge for Year 6?
- Nord Anglia International School (Dubai) – Dh85,032
- Kings School Al Barsha (Dubai) – Dh71,905
- Brighton College Abu Dhabi - Dh68,560
- Jumeirah English Speaking School (Dubai) – Dh59,728
- Gems Wellington International School – Dubai Branch – Dh58,488
- The British School Al Khubairat (Abu Dhabi) - Dh54,170
- Dubai English Speaking School – Dh51,269
*Annual tuition fees covering the 2024/2025 academic year
Summer special
FROM%20THE%20ASHES
%3Cp%3EDirector%3A%20Khalid%20Fahad%3C%2Fp%3E%0A%3Cp%3EStarring%3A%20Shaima%20Al%20Tayeb%2C%20Wafa%20Muhamad%2C%20Hamss%20Bandar%3C%2Fp%3E%0A%3Cp%3ERating%3A%203%2F5%3C%2Fp%3E%0A
The Vile
Starring: Bdoor Mohammad, Jasem Alkharraz, Iman Tarik, Sarah Taibah
Director: Majid Al Ansari
Rating: 4/5
Company Fact Box
Company name/date started: Abwaab Technologies / September 2019
Founders: Hamdi Tabbaa, co-founder and CEO. Hussein Alsarabi, co-founder and CTO
Based: Amman, Jordan
Sector: Education Technology
Size (employees/revenue): Total team size: 65. Full-time employees: 25. Revenue undisclosed
Stage: early-stage startup
Investors: Adam Tech Ventures, Endure Capital, Equitrust, the World Bank-backed Innovative Startups SMEs Fund, a London investment fund, a number of former and current executives from Uber and Netflix, among others.
if you go
No%20Windmills%20in%20Basra
%3Cp%3EAuthor%3A%20Diaa%20Jubaili%3C%2Fp%3E%0A%3Cp%3EPages%3A%20180%3C%2Fp%3E%0A%3Cp%3EPublisher%3A%20Deep%20Vellum%20Publishing%C2%A0%3C%2Fp%3E%0A
STAY%2C%20DAUGHTER
%3Cp%3E%3Cstrong%3EAuthor%3A%20%3C%2Fstrong%3EYasmin%20Azad%3C%2Fp%3E%0A%3Cp%3E%3Cstrong%3EPublisher%3A%20%3C%2Fstrong%3ESwift%20Press%3C%2Fp%3E%0A%3Cp%3E%3Cstrong%3EAvailable%3A%20%3C%2Fstrong%3ENow%3C%2Fp%3E%0A
UAE currency: the story behind the money in your pockets
THE SIXTH SENSE
Starring: Bruce Willis, Toni Collette, Hayley Joel Osment
Director: M. Night Shyamalan
Rating: 5/5
COMPANY%20PROFILE
%3Cp%3E%3Cstrong%3EName%3A%20%3C%2Fstrong%3ESmartCrowd%0D%3Cbr%3E%3Cstrong%3EStarted%3A%20%3C%2Fstrong%3E2018%0D%3Cbr%3E%3Cstrong%3EFounder%3A%20%3C%2Fstrong%3ESiddiq%20Farid%20and%20Musfique%20Ahmed%0D%3Cbr%3E%3Cstrong%3EBased%3A%20%3C%2Fstrong%3EDubai%0D%3Cbr%3E%3Cstrong%3ESector%3A%20%3C%2Fstrong%3EFinTech%20%2F%20PropTech%0D%3Cbr%3E%3Cstrong%3EInitial%20investment%3A%20%3C%2Fstrong%3E%24650%2C000%0D%3Cbr%3E%3Cstrong%3ECurrent%20number%20of%20staff%3A%3C%2Fstrong%3E%2035%0D%3Cbr%3E%3Cstrong%3EInvestment%20stage%3A%20%3C%2Fstrong%3ESeries%20A%0D%3Cbr%3E%3Cstrong%3EInvestors%3A%20%3C%2Fstrong%3EVarious%20institutional%20investors%20and%20notable%20angel%20investors%20(500%20MENA%2C%20Shurooq%2C%20Mada%2C%20Seedstar%2C%20Tricap)%3C%2Fp%3E%0A
MEDIEVIL%20(1998)
%3Cp%3E%3Cstrong%3EDeveloper%3A%3C%2Fstrong%3E%20SCE%20Studio%20Cambridge%3Cbr%3E%3Cstrong%3EPublisher%3A%3C%2Fstrong%3E%20Sony%20Computer%20Entertainment%3Cbr%3E%3Cstrong%3EConsole%3A%3C%2Fstrong%3E%20PlayStation%2C%20PlayStation%204%20and%205%3Cbr%3E%3Cstrong%3ERating%3A%3C%2Fstrong%3E%203.5%2F5%3C%2Fp%3E%0A
Results
5pm: Maiden (PA) Dh80,000 (Turf) 1,200m. Winner: Majd Al Megirat, Sam Hitchcott (jockey), Ahmed Al Shehhi (trainer)
5.30pm: Handicap (PA) Dh80,000 (T) 1,600m. Winner: Dassan Da, Patrick Cosgrave, Helal Al Alawi
6pm: Abu Dhabi Fillies Classic Prestige (PA) Dh110,000 (T) 1,400m. Winner: Heba Al Wathba, Richard Mullen, Jean de Roualle
6.30pm: Abu Dhabi Colts Classic Prestige (PA) Dh110,000 (T) 1,400m. Winner: Hameem, Adrie de Vries, Abdallah Al Hammadi
7pm: Wathba Stallions Cup Handicap (PA) Dh70,000 (T) 2,200m. Winner: Jawal Al Reef, Richard Mullen, Ahmed Al Mehairbi
Handicap (TB) Dh100,000 (T) 2,200m. Winner: Harbour Spirit, Adrie de Vries, Jaber Ramadhan.
Specs
Engine: Electric motor generating 54.2kWh (Cooper SE and Aceman SE), 64.6kW (Countryman All4 SE)
Power: 218hp (Cooper and Aceman), 313hp (Countryman)
Torque: 330Nm (Cooper and Aceman), 494Nm (Countryman)
On sale: Now
Price: From Dh158,000 (Cooper), Dh168,000 (Aceman), Dh190,000 (Countryman)
Red flags
- Promises of high, fixed or 'guaranteed' returns.
- Unregulated structured products or complex investments often used to bypass traditional safeguards.
- Lack of clear information, vague language, no access to audited financials.
- Overseas companies targeting investors in other jurisdictions - this can make legal recovery difficult.
- Hard-selling tactics - creating urgency, offering 'exclusive' deals.
Courtesy: Carol Glynn, founder of Conscious Finance Coaching
SPECS
%3Cp%3E%3Cstrong%3EEngine%3C%2Fstrong%3E%3A%202-litre%20direct%20injection%20turbo%20%0D%3Cbr%3E%3Cstrong%3ETransmission%3C%2Fstrong%3E%3A%207-speed%20automatic%20%0D%3Cbr%3E%3Cstrong%3EPower%3C%2Fstrong%3E%3A%20261hp%20%0D%3Cbr%3E%3Cstrong%3ETorque%3C%2Fstrong%3E%3A%20400Nm%20%0D%3Cbr%3E%3Cstrong%3EPrice%3C%2Fstrong%3E%3A%20From%20Dh134%2C999%26nbsp%3B%3C%2Fp%3E%0A
Globalization and its Discontents Revisited
Joseph E. Stiglitz
W. W. Norton & Company
UAE currency: the story behind the money in your pockets
Some of Darwish's last words
"They see their tomorrows slipping out of their reach. And though it seems to them that everything outside this reality is heaven, yet they do not want to go to that heaven. They stay, because they are afflicted with hope." - Mahmoud Darwish, to attendees of the Palestine Festival of Literature, 2008
His life in brief: Born in a village near Galilee, he lived in exile for most of his life and started writing poetry after high school. He was arrested several times by Israel for what were deemed to be inciteful poems. Most of his work focused on the love and yearning for his homeland, and he was regarded the Palestinian poet of resistance. Over the course of his life, he published more than 30 poetry collections and books of prose, with his work translated into more than 20 languages. Many of his poems were set to music by Arab composers, most significantly Marcel Khalife. Darwish died on August 9, 2008 after undergoing heart surgery in the United States. He was later buried in Ramallah where a shrine was erected in his honour.
MATCH INFO
Uefa Champions League final:
Who: Real Madrid v Liverpool
Where: NSC Olimpiyskiy Stadium, Kiev, Ukraine
When: Saturday, May 26, 10.45pm (UAE)
TV: Match on BeIN Sports
Real estate tokenisation project
Dubai launched the pilot phase of its real estate tokenisation project last month.
The initiative focuses on converting real estate assets into digital tokens recorded on blockchain technology and helps in streamlining the process of buying, selling and investing, the Dubai Land Department said.
Dubai’s real estate tokenisation market is projected to reach Dh60 billion ($16.33 billion) by 2033, representing 7 per cent of the emirate’s total property transactions, according to the DLD.
Company%20profile%20
%3Cp%3E%3Cstrong%3EName%3A%20%3C%2Fstrong%3EYodawy%3Cbr%3E%3Cstrong%3EBased%3A%3C%2Fstrong%3E%20Egypt%3Cbr%3E%3Cstrong%3EFounders%3A%20%3C%2Fstrong%3EKarim%20Khashaba%2C%20Sherief%20El-Feky%20and%20Yasser%20AbdelGawad%3Cstrong%3E%3Cbr%3ESector%3A%20%3C%2Fstrong%3EHealthTech%3Cbr%3E%3Cstrong%3ETotal%20funding%3A%20%3C%2Fstrong%3E%2424.5%20million%3Cbr%3E%3Cstrong%3EInvestors%3A%20%3C%2Fstrong%3EAlgebra%20Ventures%2C%20Global%20Ventures%2C%20MEVP%20and%20Delivery%20Hero%20Ventures%2C%20among%20others%3Cstrong%3E%3Cbr%3ENumber%20of%20employees%3A%3C%2Fstrong%3E%20500%3Cbr%3E%3C%2Fp%3E%0A
The years Ramadan fell in May
The specs: 2019 BMW i8 Roadster
Price, base: Dh708,750
Engine: 1.5L three-cylinder petrol, plus 11.6 kWh lithium-ion battery
Transmission: Six-speed automatic
Power: 374hp (total)
Torque: 570Nm (total)
Fuel economy, combined: 2.0L / 100km