There must be wider access to health care if a surge in the number of cancer cases in the UAE is to be reversed, experts said.
That was among the chief findings of soon-to-be-published research in The Lancet Oncology, which was responding to the latest figures, released earlier this year, which showed a 60 per cent rise in newly-diagnosed cases between 2019-23.
The series paper, titled “Cancer Control in the United Arab Emirates,” co-written by leading UAE-based oncologists and global experts, called for an urgent and comprehensive national strategy to address rising cases, inequities in care and preventive services not being used enough.
The latest figures, released by the Ministry of Health and Prevention earlier this year, showed 7,487 new incidents of cancer were found in 2023, up from 4,633 newly diagnosed cases in 2019 and 5,830 in 2021.
Due to the variation in insurance policies and approvals, access to early detection and screening campaigns can be a limiting factor
Dr Moustafa Aldaly,
oncology consultant, International Modern Hospital, Dubai
The figures come amid a growing population, but also due to relatively high obesity and smoking rates. Professor Humaid Al Shamsi, a leading medical oncologist in the UAE and visiting professor at Harvard University is the senior author of the study.
“Equity must be the cornerstone of cancer control,” said Prof Al Shamsi, who is head of Emirates Oncology Society.
“If we don't address disparities now, outcomes will worsen and costs will rise. We have the tools, talent and vision – now, we need co-ordinated execution to become a global leader in equitable, high-quality cancer care.”
Barriers to addressing the increased number of cases include low awareness, cultural stigma, limited insurance coverage for expatriates and lack of digital follow-up systems.
As the fifth leading case of death in the UAE, cancer is responsible for about eight per cent of all deaths. An ageing population, lifestyle-related risk factors such as obesity and smoking and better diagnostic capabilities have contributed to the sharp increase in cases, experts said.
The economic impact is also significant with cancer costing the UAE about Dh39.9 billion each year in treatments and lost productivity, about 2.7 per cent of GDP, Prof Al Shamsi said.
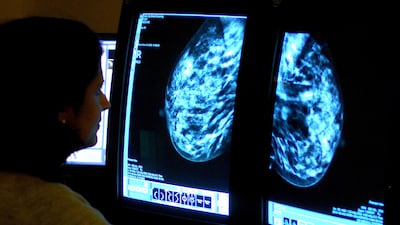
In the most recent National Cancer Registry figures from 2023, 94.8 per cent of cases were classified as invasive, or malignant. The majority of cancers, 56 per cent, were found in women, with 1,736 new cases found in the local Emirati population.
“When we try to interpret these figures we should not forget that more than 75 per cent of the population is expatriate, with different genetics, environmental exposures and also different cancer disease profiles,” said Dr Moustafa Aldaly, an oncology consultant at International Modern Hospital, Dubai.
“The main concern in the paper is about equality of cancer services, which I totally agree with. There is a need for national guidelines, and a national insurance code for cancer management. Due to the variation in insurance policies and approvals, access to early detection and screening campaigns can be a limiting factor.”
Lack of recovery networks
A lack of nationwide integration, home-care options and trained professionals were limiting the effectiveness of palliative care for cancer patients, the report found.
There was also an urgent need for more programmes providing follow up care and monitoring in recovering patients, according to the study’s co-author Dr Deborah Mukherji.
“The cancer journey doesn't end with treatment,” said Dr Mukherji, a consultant oncologist at Clemenceau Medical Centre Hospital in Dubai.
“We must build survivorship and palliative models that reflect the needs of both citizens and expatriates.”
Tackling the problem
The UAE’s cancer care landscape has grown significantly in recent years. In Dubai, the Basmah programme uses pooled insurance premiums to fund cancer treatments for expatriates who exceed their policy limits.
Now, there are more than 30 centres nationwide and five major comprehensive cancer centres but experts said there remained a variation in quality of care, particularly in more rural areas.
Due to open in 2026, the Hamdan Bin Rashid Cancer Hospital in Dubai will be the UAE’s first public comprehensive oncology hospital. It is expected to improve access to care, centralise expertise and increase the number of cancer specialists, especially surgical oncologists.
At the beginning of 2025, mandatory health insurance rolled out across the Northern Emirates.
Global pattern
While cancer survival rates continue to improve resulting from new drug combinations and more accurate blood testing, more people are being diagnosed worldwide.
According to Cancer Research in the UK, the number of people being diagnosed has increased by half in the past 50 years.
In 1973, about 413 people were diagnosed in every 100,000, but that number has also soared to about 607 per 100,000 in 2023, largely due to better diagnostics.
However, an NHS vaccination campaign for HPV, the virus related to cervical cancer, has been dealt a serious blow in recent years.
According to the UK Health Security Agency (UKHSA) more than a quarter of eligible children are missing out on the vaccine.
In contrast, the UAE has led the region in its approach to HPV and vaccinations.
Since its 2008 launch in Abu Dhabi and subsequent national roll-out, the programme achieved 82 per cent coverage in girls aged 13–14 by 2022.
While breast cancer campaigns such as the Pink Caravan continue to boost breast cancer awareness, experts called for a similar national strategy for other cancers like colorectal and lung, particularly targeting non-nationals.
Dr Neil Nijhawan, a consultant in hospice and palliative medicine at Burjeel Medical City in Abu Dhabi said compassion must be at the core of all health care.
“Palliative care, which relieves suffering and supports quality of life, remains underdeveloped in much of the region,” he said.
“Too often, patients with terminal illness receive invasive hospital treatments rather than comfort-focused care surrounded by family.
“Compassionate care isn’t sentimental – it is clinically effective as it improves communication, patient outcomes, and reduces costs.
“In contrast, systems driven more by profit than people can lead to over treatment, distress, and moral injury for both patients and clinicians.
“The UAE can lead not just in medical technology, but in compassionate innovation – by funding palliative care, supporting hospice services, and training professionals in holistic care.
“This isn’t just good healthcare policy – it’s a moral obligation.”
Company profile
Name: Dukkantek
Started: January 2021
Founders: Sanad Yaghi, Ali Al Sayegh and Shadi Joulani
Based: UAE
Number of employees: 140
Sector: B2B Vertical SaaS(software as a service)
Investment: $5.2 million
Funding stage: Seed round
Investors: Global Founders Capital, Colle Capital Partners, Wamda Capital, Plug and Play, Comma Capital, Nowais Capital, Annex Investments and AMK Investment Office
About Okadoc
Date started: Okadoc, 2018
Founder/CEO: Fodhil Benturquia
Based: Dubai, UAE
Sector: Healthcare
Size: (employees/revenue) 40 staff; undisclosed revenues recording “double-digit” monthly growth
Funding stage: Series B fundraising round to conclude in February
Investors: Undisclosed
Profile
Co-founders of the company: Vilhelm Hedberg and Ravi Bhusari
Launch year: In 2016 ekar launched and signed an agreement with Etihad Airways in Abu Dhabi. In January 2017 ekar launched in Dubai in a partnership with the RTA.
Number of employees: Over 50
Financing stage: Series B currently being finalised
Investors: Series A - Audacia Capital
Sector of operation: Transport
The%20specs%3A%20Panamera%20Turbo%20E-Hybrid
%3Cp%3E%3Cstrong%3EEngine%3A%20%3C%2Fstrong%3E4.0-litre%20twin-turbo%20V8%20hybrid%0D%3Cbr%3E%3Cstrong%3EPower%3A%20%3C%2Fstrong%3E680hp%0D%3Cbr%3E%3Cstrong%3ETorque%3A%20%3C%2Fstrong%3E930Nm%0D%3Cbr%3E%3Cstrong%3ETransmission%3A%20%3C%2Fstrong%3EEight-speed%20dual-clutch%20auto%0D%3Cbr%3E%3Cstrong%3EPrice%3A%20%3C%2Fstrong%3EFrom%20Dh749%2C000%0D%3Cbr%3E%3Cstrong%3EOn%20sale%3A%20%3C%2Fstrong%3ENow%3C%2Fp%3E%0A
The%20specs%3A%202024%20Panamera
%3Cp%3E%3Cstrong%3EEngine%3A%20%3C%2Fstrong%3E2.9-litre%20twin-turbo%20V6%0D%3Cbr%3E%3Cstrong%3EPower%3A%20%3C%2Fstrong%3E353hp%0D%3Cbr%3E%3Cstrong%3ETorque%3A%20%3C%2Fstrong%3E500Nm%0D%3Cbr%3E%3Cstrong%3ETransmission%3A%20%3C%2Fstrong%3EEight-speed%20dual-clutch%20auto%0D%3Cbr%3E%3Cstrong%3EPrice%3A%20%3C%2Fstrong%3EFrom%20Dh408%2C200%0D%3Cbr%3E%3Cstrong%3EOn%20sale%3A%3C%2Fstrong%3E%20Now%3C%2Fp%3E%0A
THE SPECS
Engine: 6.75-litre twin-turbocharged V12 petrol engine
Power: 420kW
Torque: 780Nm
Transmission: 8-speed automatic
Price: From Dh1,350,000
On sale: Available for preorder now
KEY HIGHLIGHTS
Healthcare spending to double to $2.2 trillion rupees
Launched a 641billion-rupee federal health scheme
Allotted 200 billion rupees for the recapitalisation of state-run banks
Around 1.75 trillion rupees allotted for privatisation and stake sales in state-owned assets
Electric scooters: some rules to remember
- Riders must be 14-years-old or over
- Wear a protective helmet
- Park the electric scooter in designated parking lots (if any)
- Do not leave electric scooter in locations that obstruct traffic or pedestrians
- Solo riders only, no passengers allowed
- Do not drive outside designated lanes
Specs
Engine: Duel electric motors
Power: 659hp
Torque: 1075Nm
On sale: Available for pre-order now
Price: On request
Keep it fun and engaging
Stuart Ritchie, director of wealth advice at AES International, says children cannot learn something overnight, so it helps to have a fun routine that keeps them engaged and interested.
“I explain to my daughter that the money I draw from an ATM or the money on my bank card doesn’t just magically appear – it’s money I have earned from my job. I show her how this works by giving her little chores around the house so she can earn pocket money,” says Mr Ritchie.
His daughter is allowed to spend half of her pocket money, while the other half goes into a bank account. When this money hits a certain milestone, Mr Ritchie rewards his daughter with a small lump sum.
He also recommends books that teach the importance of money management for children, such as The Squirrel Manifesto by Ric Edelman and Jean Edelman.
COMPANY PROFILE
Name: HyperSpace
Started: 2020
Founders: Alexander Heller, Rama Allen and Desi Gonzalez
Based: Dubai, UAE
Sector: Entertainment
Number of staff: 210
Investment raised: $75 million from investors including Galaxy Interactive, Riyadh Season, Sega Ventures and Apis Venture Partners
Cases of coronavirus in the GCC as of March 15
Saudi Arabia – 103 infected, 0 dead, 1 recovered
UAE – 86 infected, 0 dead, 23 recovered
Bahrain – 210 infected, 0 dead, 44 recovered
Kuwait – 104 infected, 0 dead, 5 recovered
Qatar – 337 infected, 0 dead, 4 recovered
Oman – 19 infected, 0 dead, 9 recovered
How to apply for a drone permit
- Individuals must register on UAE Drone app or website using their UAE Pass
- Add all their personal details, including name, nationality, passport number, Emiratis ID, email and phone number
- Upload the training certificate from a centre accredited by the GCAA
- Submit their request
What are the regulations?
- Fly it within visual line of sight
- Never over populated areas
- Ensure maximum flying height of 400 feet (122 metres) above ground level is not crossed
- Users must avoid flying over restricted areas listed on the UAE Drone app
- Only fly the drone during the day, and never at night
- Should have a live feed of the drone flight
- Drones must weigh 5 kg or less
MATCH INFO
Uefa Champions League quarter-final, second leg (first-leg score):
Manchester City (0) v Tottenham Hotspur (1), Wednesday, 11pm UAE
Match is on BeIN Sports
UAE currency: the story behind the money in your pockets
GAC GS8 Specs
Engine: 2.0-litre 4cyl turbo
Power: 248hp at 5,200rpm
Torque: 400Nm at 1,750-4,000rpm
Transmission: 8-speed auto
Fuel consumption: 9.1L/100km
On sale: Now
Price: From Dh149,900
Brief scores:
Scotland 371-5, 50 overs (C MacLeod 140 no, K Coetzer 58, G Munsey 55)
England 365 all out, 48.5 overs (J Bairstow 105, A Hales 52; M Watt 3-55)
Result: Scotland won by six runs
Winners
Ballon d’Or (Men’s)
Ousmane Dembélé (Paris Saint-Germain / France)
Ballon d’Or Féminin (Women’s)
Aitana Bonmatí (Barcelona / Spain)
Kopa Trophy (Best player under 21 – Men’s)
Lamine Yamal (Barcelona / Spain)
Best Young Women’s Player
Vicky López (Barcelona / Spain)
Yashin Trophy (Best Goalkeeper – Men’s)
Gianluigi Donnarumma (Paris Saint-Germain and Manchester City / Italy)
Best Women’s Goalkeeper
Hannah Hampton (England / Aston Villa and Chelsea)
Men’s Coach of the Year
Luis Enrique (Paris Saint-Germain)
Women’s Coach of the Year
Sarina Wiegman (England)
More from Rashmee Roshan Lall
Company profile
Date started: 2015
Founder: John Tsioris and Ioanna Angelidaki
Based: Dubai
Sector: Online grocery delivery
Staff: 200
Funding: Undisclosed, but investors include the Jabbar Internet Group and Venture Friends
Wicked: For Good
Director: Jon M Chu
Starring: Ariana Grande, Cynthia Erivo, Jonathan Bailey, Jeff Goldblum, Michelle Yeoh, Ethan Slater
Rating: 4/5
Specs%3A%202024%20McLaren%20Artura%20Spider
%3Cp%3E%3Cstrong%3EEngine%3A%3C%2Fstrong%3E%203.0-litre%20twin-turbo%20V6%20and%20electric%20motor%3Cbr%3E%3Cstrong%3EMax%20power%3A%3C%2Fstrong%3E%20700hp%20at%207%2C500rpm%3Cbr%3E%3Cstrong%3EMax%20torque%3A%3C%2Fstrong%3E%20720Nm%20at%202%2C250rpm%3Cbr%3E%3Cstrong%3ETransmission%3A%3C%2Fstrong%3E%20Eight-speed%20dual-clutch%20auto%3Cbr%3E%3Cstrong%3E0-100km%2Fh%3A%3C%2Fstrong%3E%203.0sec%3Cbr%3E%3Cstrong%3ETop%20speed%3A%20%3C%2Fstrong%3E330kph%3Cbr%3E%3Cstrong%3EPrice%3A%3C%2Fstrong%3E%20From%20Dh1.14%20million%20(%24311%2C000)%3Cbr%3E%3Cstrong%3EOn%20sale%3A%3C%2Fstrong%3E%20Now%3C%2Fp%3E%0A
COMPANY%20PROFILE
%3Cp%3E%3Cstrong%3EName%3A%20%3C%2Fstrong%3ESmartCrowd%0D%3Cbr%3E%3Cstrong%3EStarted%3A%20%3C%2Fstrong%3E2018%0D%3Cbr%3E%3Cstrong%3EFounder%3A%20%3C%2Fstrong%3ESiddiq%20Farid%20and%20Musfique%20Ahmed%0D%3Cbr%3E%3Cstrong%3EBased%3A%20%3C%2Fstrong%3EDubai%0D%3Cbr%3E%3Cstrong%3ESector%3A%20%3C%2Fstrong%3EFinTech%20%2F%20PropTech%0D%3Cbr%3E%3Cstrong%3EInitial%20investment%3A%20%3C%2Fstrong%3E%24650%2C000%0D%3Cbr%3E%3Cstrong%3ECurrent%20number%20of%20staff%3A%3C%2Fstrong%3E%2035%0D%3Cbr%3E%3Cstrong%3EInvestment%20stage%3A%20%3C%2Fstrong%3ESeries%20A%0D%3Cbr%3E%3Cstrong%3EInvestors%3A%20%3C%2Fstrong%3EVarious%20institutional%20investors%20and%20notable%20angel%20investors%20(500%20MENA%2C%20Shurooq%2C%20Mada%2C%20Seedstar%2C%20Tricap)%3C%2Fp%3E%0A
THE%20SPECS
%3Cp%3EBattery%3A%2060kW%20lithium-ion%20phosphate%3Cbr%3EPower%3A%20Up%20to%20201bhp%3Cbr%3E0%20to%20100kph%3A%207.3%20seconds%3Cbr%3ERange%3A%20418km%3Cbr%3EPrice%3A%20From%20Dh149%2C900%3Cbr%3EAvailable%3A%20Now%3C%2Fp%3E%0A
Four motivational quotes from Alicia's Dubai talk
“The only thing we need is to know that we have faith. Faith and hope in our own dreams. The belief that, when we keep going we’re going to find our way. That’s all we got.”
“Sometimes we try so hard to keep things inside. We try so hard to pretend it’s not really bothering us. In some ways, that hurts us more. You don’t realise how dishonest you are with yourself sometimes, but I realised that if I spoke it, I could let it go.”
“One good thing is to know you’re not the only one going through it. You’re not the only one trying to find your way, trying to find yourself, trying to find amazing energy, trying to find a light. Show all of yourself. Show every nuance. All of your magic. All of your colours. Be true to that. You can be unafraid.”
“It’s time to stop holding back. It’s time to do it on your terms. It’s time to shine in the most unbelievable way. It’s time to let go of negativity and find your tribe, find those people that lift you up, because everybody else is just in your way.”